Understanding Arthritis: Treatments and Management
Arthritis refers to a group of conditions characterized by inflammation and stiffness in the joints,
causing pain and reduced mobility. It is a common chronic health issue affecting millions worldwide,
with various types such as osteoarthritis (OA), rheumatoid arthritis (RA), and gout. Effective
treatment and management strategies play a crucial role in improving symptoms and enhancing quality
of life for individuals living with arthritis.
Types of Arthritis
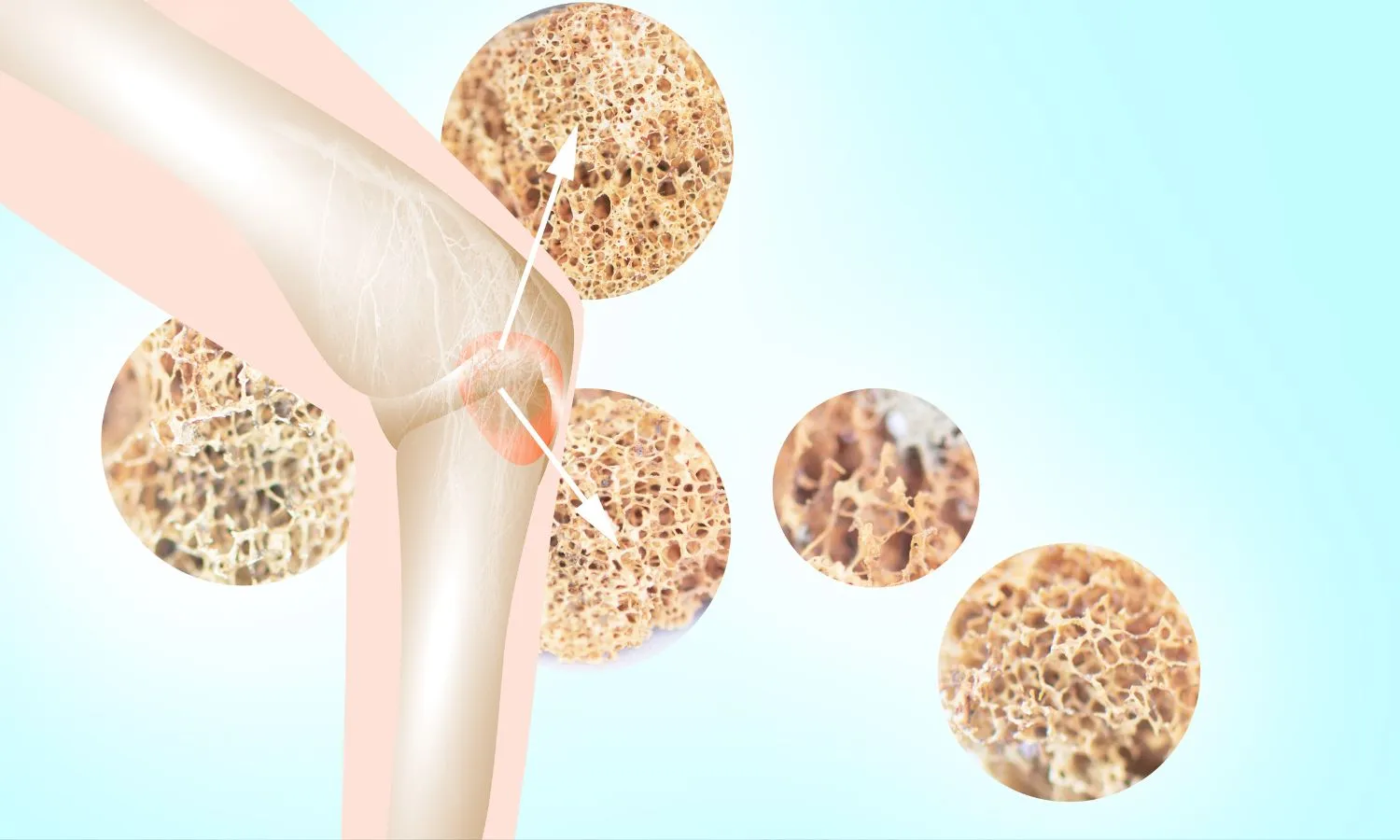
1. Osteoarthritis (OA):
OA is the most prevalent form of arthritis, typically occurring due to
wear and tear on joints over time. It commonly affects weight-bearing joints such as knees, hips,
and spine, causing pain, stiffness, and reduced range of motion.
2. Rheumatoid Arthritis (RA):
RA is an autoimmune disorder where the immune system mistakenly attacks the synovium (lining of
joints), leading to inflammation, pain, and joint damage. It can affect multiple joints
simultaneously and may also cause systemic symptoms like fatigue and fever.
3. Gout:
Gout is characterized by sudden, severe attacks of pain, redness, and swelling in joints, often the
big toe. It occurs due to the build-up of uric acid crystals in the joints and is more common in
men.
Treatment Approaches
1. Medications:
Immediate treatment often includes rest to prevent further damage and
application of ice to reduce swelling and inflammation.
- Pain Relievers (Analgesics): Over-the-counter options like acetaminophen or
prescription-strength NSAIDs (nonsteroidal anti-inflammatory drugs) such as ibuprofen help
manage pain and inflammation.
- Disease-Modifying Antirheumatic Drugs (DMARDs): These medications, like
methotrexate or biologics, are used to treat autoimmune forms of arthritis like RA by
suppressing the immune system's abnormal response.
- Corticosteroids: Injections of corticosteroids into affected joints provide
rapid relief from inflammation and pain, particularly useful during flare-ups.
2. Physical Therapy:
Customized exercise programs designed by physical therapists help
improve joint function, strengthen muscles around affected joints, and maintain flexibility.
Low-impact activities like swimming or cycling are often recommended to reduce stress on joints.
3. Lifestyle Modifications:
- Weight Management: Maintaining a healthy weight reduces stress on
weight-bearing joints, alleviating symptoms of osteoarthritis (OA).
- Joint Protection: Using assistive devices such as braces or splints can support
joints and reduce strain during daily activities.
- Corticosteroids: Injections of corticosteroids into affected joints provide
rapid relief from inflammation and pain, particularly useful during flare-ups.
- Balanced Diet: Certain foods, like those rich in omega-3 fatty acids (found in
fish) or antioxidants (found in fruits and vegetables), may help reduce inflammation associated
with arthritis.
Surgical Interventions:
- Joint Replacement: In severe cases of OA, hip or knee replacement surgery may
be recommended to replace damaged joints with prosthetic implants, relieving pain and restoring
function.
- Joint Fusion: For rheumatoid arthritis (RA) or severe arthritis in smaller
joints like wrists or ankles, joint fusion surgery may be performed to stabilize and relieve
pain.
Management Strategies
- Education and Self-Management: Understanding arthritis and its management
empowers individuals to participate actively in their care. Learning about symptoms, treatments,
and lifestyle adjustments helps in making informed decisions and improving overall well-being.
- Regular Monitoring: Routine check-ups with healthcare providers are essential
for monitoring disease progression, evaluating treatment effectiveness, and adjusting
medications or therapies as needed.
- Emotional Support: Living with chronic pain and mobility challenges can impact
mental health. Support groups, counseling, or therapy can provide emotional support and
strategies for coping with arthritis-related stress.